Chiropractic ABN’s

Welcome to Billing Buddies YouTube and Podcast series.
In this episode, we will be discussing Chiropractic ABNs.
First, let’s define an ABN. An ABN is an abbreviation of a Medicare form known as the Advanced Beneficiary Notice. Medicare requires providers give an ABN to beneficiaries if the Medicare services they are proposing to deliver is suspected to not be covered by Medicare. If the service is statutorily excluded from the Medicare program, such as exams and therapies for chiropractic care, Medicare does not require an ABN be presented to the patient. Medicare only requires an ABN be presented on services that can be covered under the program such as CMT’s for chiropractic care.
It’s very important when receiving information that you can look up and research the data yourself. For this reason, whenever possible, Billing Buddies will share the source for you to review. The information from this presentation came from www.CMS.gov. You can type ABN in the upper right-hand corner of the screen and search for information on Advance Beneficiary Notices or ABN’s.
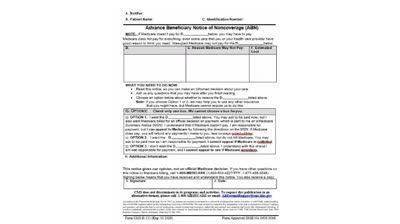
Now, let’s take a look at the form. There are several boxes to complete. You can see items A through J are to be completed by the provider and the patient. Let’s review the form.
Field A = Enter the Notifiers Information – This is the clinic and staff member presenting the ABN.
Field B = Enter the Patient’s Name
Field C = Enter the Patient’s Medicare Number
Field D = Enter the Service to be provided. In Chiropractic care, this would be the CMT. You could enter codes 98940 – 98942 in this field.
Field E = Enter the Reason Medicare may not pay. In Chiropractic care, the most common reason would be that the CMT was considered maintenance care. But, review your Local Coverage Determination from your carrier for a complete list.
Field F = Enter the estimated cost. If more than one service is listed in Box D, enter the estimated cost for all services.
Field G = All the fields on the ABN are important, but this one is especially important. Patient’s are required to pick one of the three options. The provider may not complete this portion of the form or it will invalidate the form.
Field H = This is a field where additional information may be provided.
Field I = This requires the patient or representative to sign the form. If a representative signs the form, have the representative write “representative” in parenthesis after his/her signature.
Field J = The patient or representative must date the form when signed.
That completes our ABN video. Thank you for watching. Please subscribe to our channel and like our videos. Also, please comment if you would like other videos presented and suggestions on topics.
Billing Buddies has been assisting providers since 1994 and offers billing services, training and consulting. For more information, call or text 612.432.2366 or email bonnie@billingbuddies.com.


Billing Buddies®